If you’re dealing with PCOS hair loss or hair loss with PCOS, you’re not alone, and you’re not imagining the strange mismatch where scalp hair feels thinner while facial or body hair seems more noticeable.
It can be upsetting, confusing, and challenging to put into words, especially when it appears to be happening gradually.
The truth is, PCOS can affect hair in more than one way, and the right next step depends on what pattern you’re seeing and what else is going on in your body.
Before jumping into products or quick fixes, it helps to pause and look at the signs your hair and scalp are giving you, because that’s what points you in the right direction.
What Is Female Pattern Hair Loss (FPHL)?
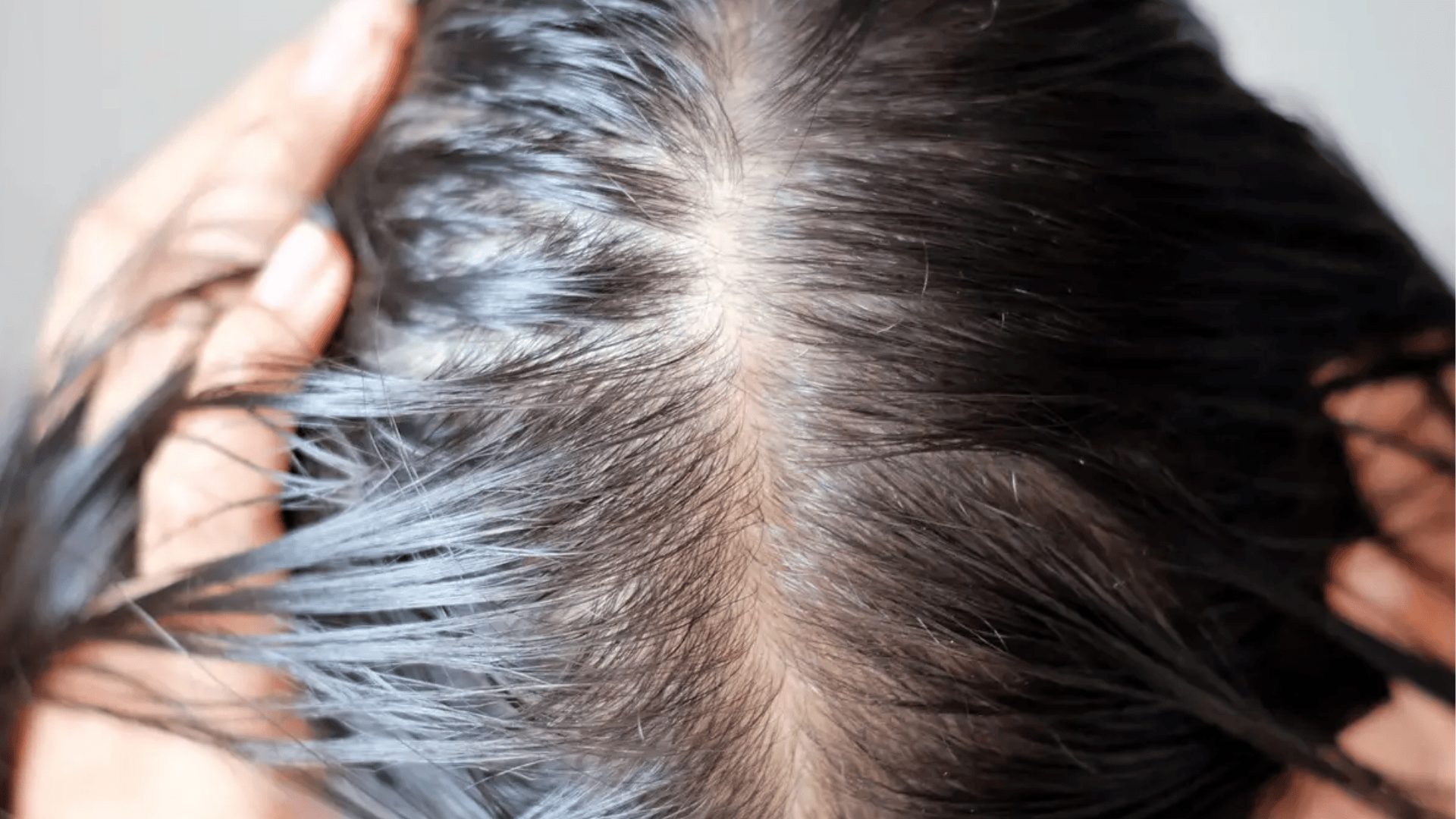
Female Pattern Hair Loss (FPHL) is a genetically influenced, progressive type of thinning that follows a recognizable pattern.
Instead of shedding evenly across the whole scalp, it often widens the part and reduces density at the crown and front of the scalp, while the hairline at the forehead may stay relatively intact.
Online, you may also see it called female androgenetic alopecia or androgenic alopecia in women; the “androgen” label reflects a hormone link, though in women it isn’t always direct.
FPHL is different from telogen effluvium, which causes diffuse, trigger-related shedding that is often temporary, and it differs from alopecia areata, which causes patchy, round bald spots in clusters.
Symptoms of FPHL With PCOS
FPHL usually shows up as gradual, patterned thinning, more about reduced density over time than sudden, dramatic shedding.
Scalp Pattern Features:
- Your center part becomes broader and more visible
- The crown and top of your scalp look “see-through” in photos or bright lighting
- Hair density decreases gradually over months or years across the top of your head
- The change happens slowly, not in dramatic shedding episodes
What You’ll Notice Day-to-Day:
- Your ponytail feels thinner when you pull your hair back
- More scalp shows through in selfies or video calls
- You might notice some shedding, but the bigger issue is reduced overall density
- The thinning becomes more evident over time, even without clumps in the shower
Key difference: FPHL is mainly patterned thinning, while telogen effluvium is mainly sudden increased shedding. Some people can have both.
Why PCOS Makes Hair Loss Worse (Causes of FPHL)
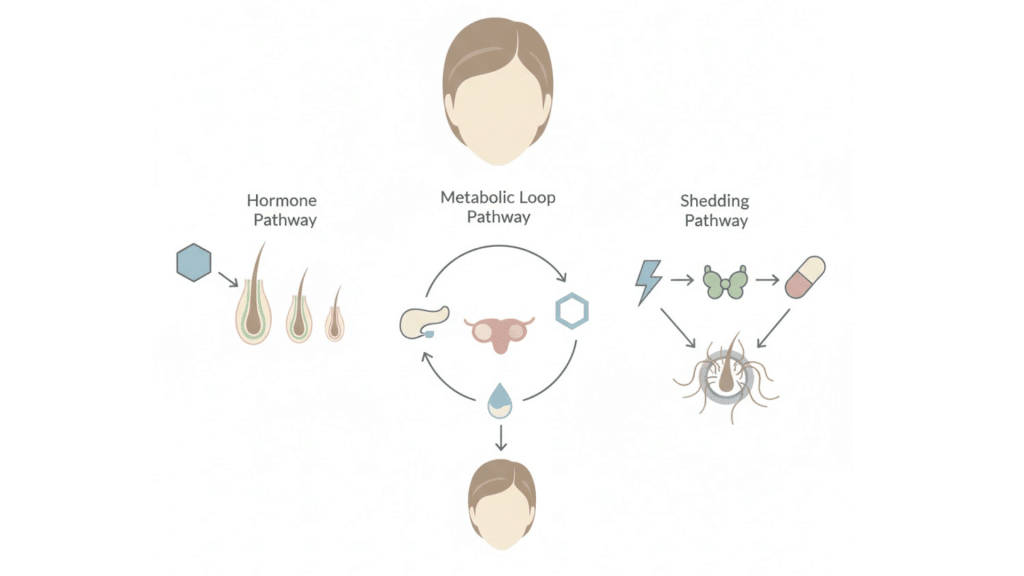
PCOS can speed up pattern thinning through hormone sensitivity, metabolic changes, and temporary shedding triggers that stack together.
1. Core Biological Drivers
FPHL develops when scalp follicles become sensitive to androgens, especially DHT. Over time, follicles shrink, strands grow finer and shorter, and growth cycles weaken until hair becomes visibly thinner.
2. The PCOS “Multiplier Effect”
PCOS often increases overall androgen activity. Insulin resistance can further raise androgen production, creating a hormonal loop that may intensify thinning and make progression feel faster or harder to control.
3. The Telogen Effluvium Overlap
Alongside FPHL, many people also experience telogen effluvium, temporary shedding triggered by stress, illness, nutrient deficiencies, or thyroid issues. This overlap can increase shedding, but TE is often more reversible.
Can Hair Loss From PCOS Be Reversed?
The honest answer is: it depends, and “reversal” can mean two different things.
First is stabilization, which means slowing or stopping further thinning and keeping the hair you still have; this is often the most realistic early goal.
Second is regrowth, which means recovering the density you’ve already lost, and that depends on how long follicles have been miniaturizing and whether they can still produce thick, visible hairs.
You typically have better odds with early action, but no option can promise a full return to pre-PCOS density.
The most reversible piece is often telogen effluvium, where triggers like stress, low iron/ferritin, vitamin D deficiency, or thyroid issues can improve within 3–6 months.
Key Factors That Influence Hair Regrowth
Hair regrowth isn’t one-size-fits-all. Your results depend on follicle health, consistency, and whether other triggers are quietly worsening thinning.
- Duration and severity of miniaturization: The longer the follicles have produced fine, wispy hairs, the harder reversal becomes.
- Treatment consistency and timeline: Hair cycles move slowly; plan on 6–12 months of steady treatment to judge progress.
- Correcting co-triggers: Fixing thyroid issues, anemia/low ferritin, or low vitamin D can significantly improve outcomes when they’re involved.
- PCOS metabolic control: Managing insulin resistance and stabilizing androgen activity supports a healthier environment for growth.
- Scalp health and hair practices: Less inflammation, less traction/heat, and fewer harsh chemicals help your efforts work better.
Small changes add up, but consistency matters most. Track progress monthly and adjust with a clinician if results stall.
Are There Tests to Diagnose FPHL?

Most people don’t need extensive testing. Diagnosis often comes from pattern recognition, with tools and labs used when something looks off.
- Diagnosis is usually clinical: Many dermatologists can diagnose FPHL from your history and scalp exam, especially with a widening part and crown thinning.
- Trichoscopy (dermoscopy): A magnified scalp exam that shows miniaturized hairs and density patterns, helping confirm FPHL and rule out similar conditions.
- Optional lab work: Thyroid tests (TSH, free T4), CBC (anemia), ferritin (iron stores), and vitamin D can help identify triggers that worsen thinning.
- When labs become more critical: If shedding is excessive, the pattern isn’t typical, or other symptoms suggest thyroid or nutrient issues.
- Staging severity: The Ludwig scale (3 grades) and Sinclair scale (5 grades) help document baseline severity and track treatment response.
Testing isn’t just about a label; it helps uncover reversible contributors and gives a clear starting point to measure real progress.
How PCOS Is Diagnosed
Since PCOS and hair loss often occur together, it’s worth understanding how doctors diagnose the underlying condition.
PCOS diagnosis typically involves evaluating your symptom pattern, menstrual history, and clinical findings.
Your doctor may order blood tests to check hormone levels, glucose, and insulin markers, or perform a pelvic ultrasound to look at ovarian morphology.
The specific criteria and testing approach vary by provider and clinical presentation, so your experience may look different from someone else’s.
The important point: getting your PCOS properly diagnosed and managed creates a better foundation for addressing hair loss.
Medical Treatments for FPHL With PCOS
These options target the most common drivers of thinning in PCOS: follicle miniaturization, androgen activity, and slow regrowth cycles, so results depend on consistency and time.
1. Topical Minoxidil (First-Line Treatment)
Minoxidil is the most studied option for female pattern thinning. It helps keep follicles in the growth phase longer and can improve density over time.
Typical use includes 5% foam once daily or 2% solution twice daily, with results judged after several months.
2. Oral Anti-Androgens (PCOS-Relevant Options)
Anti-androgens reduce the effect of androgens on hair follicles.
Spironolactone is commonly used in PCOS, often within 25–200 mg/day ranges. It requires monitoring, and pregnancy prevention is essential during use.
3. Hormonal Contraception Options
Some birth control pills contain progestins with anti-androgenic effects, which may help PCOS-related symptoms that affect hair.
Drospirenone is often discussed, while cyproterone acetate is used in some regions outside the U.S.
4. Finasteride and Dutasteride
These medications lower DHT by blocking testosterone conversion, but use in women is typically off-label and more selective.
They’re often considered for postmenopausal patients or specialist-managed cases with strict pregnancy prevention.
5. Procedural Options (Adjunct Treatments)
Procedures can support medical therapy, but usually aren’t replacements.
Platelet-Rich Plasma (PRP) involves scalp injections from your own concentrated platelets, and Low-Level Laser/Light Therapy (LLLT) uses light devices to stimulate follicles. Evidence is mixed, so expectations should stay realistic.
Home Remedies and Supportive Care
Medical treatment does the heavy lifting, but daily habits can protect fragile hair, reduce breakage, and support healthier regrowth conditions.
- Avoid tight hairstyles: Skip tight ponytails, braids, or buns that pull on the scalp (traction can worsen thinning).
- Limit heat and chemicals: Reduce frequent straightening, curling, bleaching, and harsh chemical treatments when possible.
- Be gentle when detangling: Use a wide-tooth comb on wet hair; avoid aggressive brushing or ripping through knots.
- Choose mild shampooing: If your scalp is sensitive, try gentle, sulfate-free options and avoid over-scrubbing.
- Prioritize protein: Hair is protein-based; consistent intake matters more than “hair vitamins.”
- Don’t take iron blindly: Only supplement iron if labs confirm deficiency; excess iron can cause problems.
Optional natural add-ons (limited evidence):
- Spearmint tea: Small PCOS studies suggest modest androgen-lowering effects; consider it supportive, not a standalone fix.
- Saw palmetto: Evidence is weak; may interact with medications and should be avoided in pregnancy/breastfeeding, check with your doctor.
Natural options can be supportive, but they work best alongside proven treatments, realistic timelines, and consistent, gentle routines.
When to See a Specialist
See a specialist if your hair loss is worsening quickly, you’re unsure if it’s FPHL or something else, or your scalp feels painful, itchy, scaly, or inflamed.
A dermatologist can confirm the pattern with tools like trichoscopy, document severity using the Ludwig or Sinclair scale, and track changes over time, plus discuss prescriptions, PRP, or other advanced options.
You should also see an OB-GYN or endocrinologist if your PCOS symptoms aren’t well-controlled, you have irregular periods, metabolic concerns, or signs of insulin resistance, or you need support choosing hormonal contraception.
Because PCOS affects multiple systems, coordinated care often leads to better, more sustainable results.
Making Your Decision
With PCOS hair loss,the most critical move is choosing a plan you can stick with, then giving it enough time to work.
Start by booking a dermatologist visit to confirm the pattern, set a baseline, and build a routine you’ll actually follow.
If PCOS symptoms feel unmanaged, loop in your OB-GYN or endocrinologist so your overall treatment supports your hair goals, not the opposite.
Keep expectations practical, but don’t undersell what consistency can do. Take clear photos once a month, at the same angle and with the same lighting, so that you can spot real change.
Ready to start? Make your appointment this week and write down your top three questions to bring.