Let’s be honest: compression socks used to be the fashion equivalent of a medical alert bracelet.
Beige. Bland. Prescribed for post-surgical patients, DVT prevention, and your grandmother’s varicose veins. They worked, sure; but nobody wanted to wear them.
That era is over.
Today’s compression wear has evolved into something unrecognizable: sleek performance gear engineered with graduated pressure zones, moisture-wicking fabrics, and designs that wouldn’t look out of place in an athlete’s gym bag or a traveler’s carry-on.
Runners swear by them. Flight attendants live in them. Nurses won’t work without them.
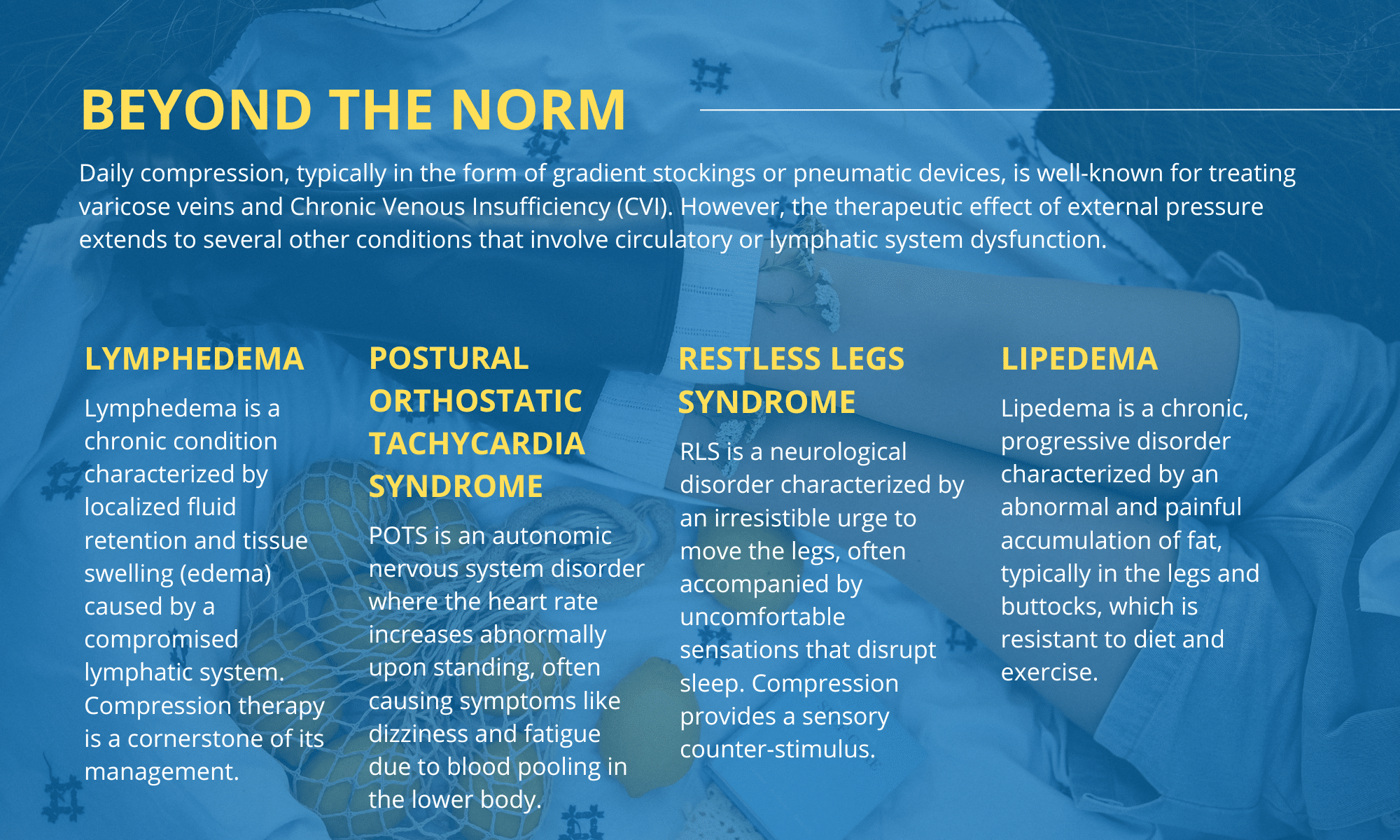
But here’s what most people don’t realize: the real magic of compression therapy isn’t just preventing swollen ankles or smoothing out bulging veins. It’s what happens beneath the surface, including improved circulation, reduced inflammation, enhanced lymphatic drainage, that makes these garments quietly revolutionary for a range of health conditions that have nothing to do with visible leg problems.
We’re talking about issues that drain your energy, mess with your focus, limit your mobility, and chip away at your quality of life. Conditions that often get dismissed as “just part of getting older” or blamed on stress and poor sleep.
This isn’t about vanity. It’s about function, recovery, and reclaiming how your body feels every single day. Here are five medical conditions where daily compression isn’t just helpful—it’s transformative.
1. Lymphedema: managing fluid buildup & swelling
Lymphedema occurs when your lymphatic system can’t adequately drain lymph fluid, typically in the arms or legs. This results in chronic swelling that can become progressively worse without intervention.
While often associated with cancer treatment or surgery, lymphedema can also be hereditary or develop from infection or injury.
Compression socks work by providing external pressure that helps push excess fluid back into circulation.
The graduated compression, tighter at the ankle and gradually loosening toward the knee—mimics the natural muscle pump action your body uses to move lymph fluid upward against gravity.
For those managing this condition, high quality medical-grade 20 30 compression socks are typically recommended as part of decongestive therapy. This level of graduated pressure is strong enough to counter fluid accumulation while still allowing safe, daily wear under medical guidance. Consistent use can significantly reduce limb circumference, prevent recurring swelling, and lower the risk of cellulitis, a common and painful complication of lymphedema.
The key is consistency. Complete Decongestive Therapy for lymphedema is a daily commitment that preserves mobility, supports lymphatic flow, and helps prevent long-term progression of the condition.
2. Chronic venous insufficiency: supporting weakened vein valves
Chronic Venous Insufficiency develops when the valves in your leg veins weaken or become damaged, making it difficult for blood to flow back toward the heart. Instead, blood pools in the lower legs, causing aching, heaviness, swelling, skin discoloration, and eventually, venous ulcers.
Unlike varicose veins (which are a symptom), CVI is the underlying vascular condition. And while surgery or other procedures may be necessary in advanced cases, compression therapy remains the gold standard for managing symptoms and preventing progression.
Medical compression socks improve venous return by applying consistent pressure that assists faulty valves in moving blood upward.
Studies have shown that wearing 20-30 mmHg compression can reduce leg swelling, alleviate pain, and accelerate healing of venous leg ulcers when used in conjunction with proper wound care.
For individuals with CVI, compression isn’t optional—it’s protective. It reduces the workload on compromised veins and helps preserve long-term leg health.
3. Plantar Fasciitis & Foot/Ankle Inflammation
While compression socks are often associated with calves and thighs, targeted compression for the foot and ankle plays a crucial role in managing plantar fasciitis, Achilles tendonitis, and general inflammatory foot conditions.
Understanding Plantar Fasciitis: This condition is characterized by stabbing heel pain, especially in the morning, and occurs when the thick band of tissue connecting your heel to your toes becomes inflamed.
How Compression Socks Help:
- Provide targeted arch support that reduces strain on the plantar fascia
- Improve circulation to deliver oxygen-rich blood to inflamed tissues
- Stabilize the arch through gentle, consistent pressure
- Reduce micro-tears in damaged tissue by limiting excessive movement
- Speed healing through enhanced blood flow and reduced inflammation
When Compression Works Best: The benefit comes from both mechanical support and enhanced blood flow. Many users experience significant pain reduction, particularly when wearing compression overnight or during long periods of standing.
Who Benefits Most:
- Athletes recovering from training injuries
- Service workers who stand for extended shifts
- Runners dealing with chronic foot pain
- Anyone with active lifestyles who can’t afford downtime
Compression socks help these individuals stay mobile and active without aggravating existing foot pain or risking further injury.
4. Diabetes-related circulation issues and neuropathy
Diabetic patients face a unique set of circulatory challenges. High blood sugar levels can damage blood vessels and nerves over time, leading to poor circulation, loss of sensation (neuropathy), slow wound healing, and increased risk of foot ulcers and infections.
Compression socks for diabetics must be chosen carefully, too much pressure can worsen circulation in cases of peripheral artery disease, but appropriate compression (typically 15-20 mmHg) can improve venous return, reduce swelling, and promote healthier legs and feet.
For diabetic neuropathy patients, compression also provides a gentle tactile reminder of foot positioning, which can improve proprioception (spatial awareness) when nerve sensation is diminished. This added awareness may help prevent injuries from bumps or missteps that go unnoticed.
Always consult with a healthcare provider before starting compression therapy if you have diabetes, especially if you have existing wounds or arterial disease. When used correctly, compression can be a valuable tool in diabetic foot care protocols.
5. POTS & Orthostatic Hypotension: Stabilizing Blood Flow When Standing
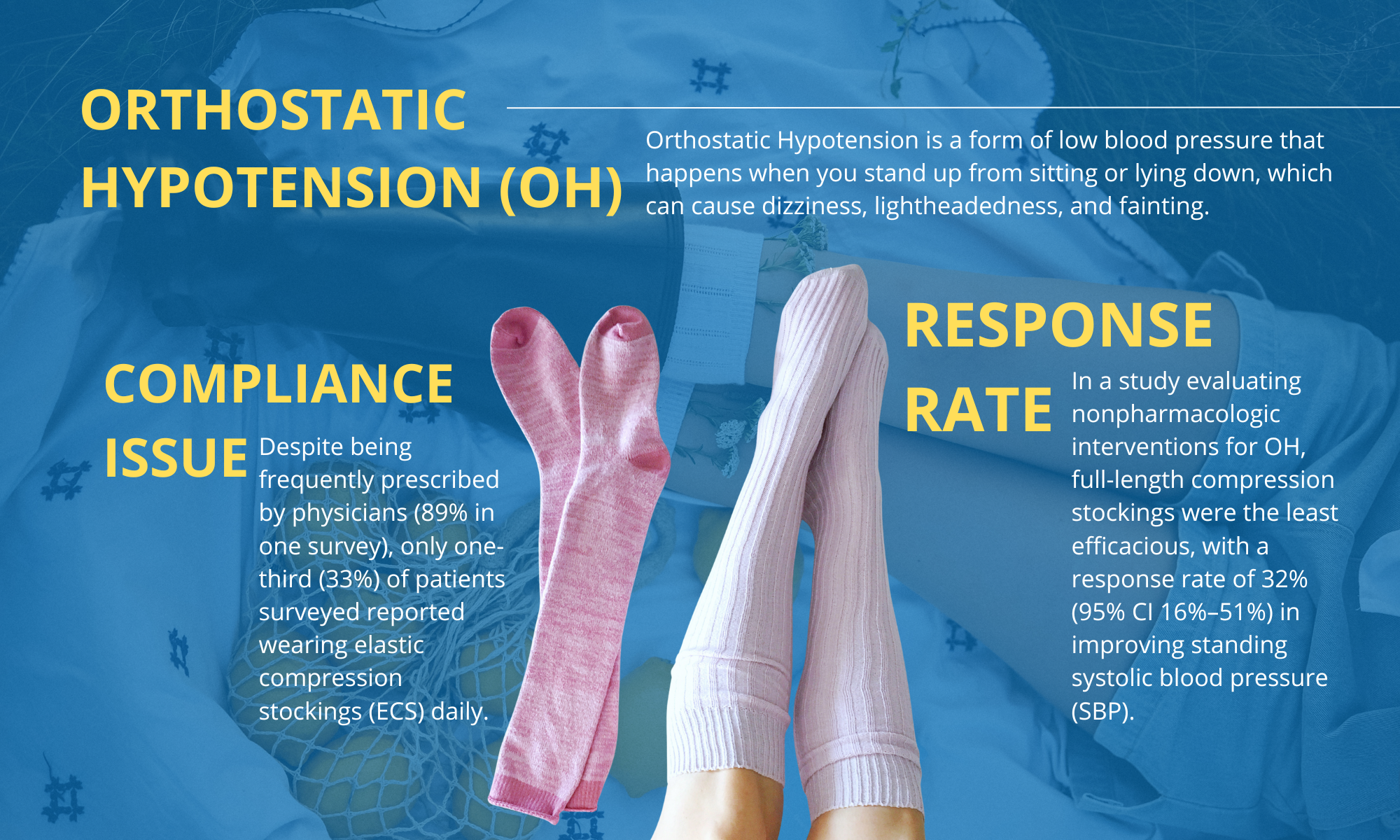
Both Postural Orthostatic Tachycardia Syndrome (POTS) and orthostatic hypotension are forms of dysautonomia where the autonomic nervous system struggles to regulate blood flow during position changes, particularly when transitioning from lying down to standing.
Understanding the Conditions:
- POTS: Characterized by rapid heart rate increase (30+ bpm), dizziness, brain fog, fatigue, and fainting spells
- Orthostatic Hypotension: Marked by significant blood pressure drop when standing, causing lightheadedness, blurred vision, weakness, and potential falls
The Common Problem: In both conditions, blood pools in the lower extremities when standing, depriving the brain and upper body of adequate circulation. This venous pooling creates debilitating symptoms that can make daily activities feel insurmountable.
How Compression Socks Help:
- Counteract venous pooling by maintaining consistent pressure on leg veins
- Encourage blood return to the heart through graduated compression (typically 20-30 mmHg)
- Reduce symptom severity including dizziness, fatigue, and cognitive dysfunction
- Prevent falls by stabilizing blood pressure during position changes
- Improve stamina for daily activities and exercise tolerance
Clinical Evidence: Combined with increased salt and fluid intake, compression therapy is frequently recommended by cardiologists and autonomic specialists as a first-line, non-pharmacological intervention for managing both POTS and orthostatic hypotension symptoms.
Finding the Right Compression: Pressure levels and fit
Not all compression socks are created equal. Pressure is measured in millimeters of mercury (mmHg), and choosing the right level depends on your specific condition:
- 8-15 mmHg: Mild compression for general leg fatigue, travel, or prevention
- 15-20 mmHg: Moderate compression for mild swelling, early varicose veins, or diabetes management
- 20-30 mmHg: Firm compression for moderate to severe swelling, CVI, POTS, or post-surgical recovery
- 30-40 mmHg+: Extra-firm medical-grade compression for lymphedema, severe CVI, or as prescribed by a physician
Proper fit is critical. Compression that’s too loose won’t deliver therapeutic benefits; too tight can restrict circulation and cause discomfort. Professional fitting or detailed measurement guides are essential for medical-grade compression.
The Bottom Line: Compression as preventive medicine
Compression therapy is a clinically validated intervention that improves circulation, reduces inflammation, supports damaged tissues, and enhances quality of life for millions dealing with chronic conditions.
Whether you’re managing lymphedema, POTS, CVI, plantar fasciitis, or diabetic complications, the right compression socks can make the difference between enduring your day and thriving through it.
Talk to your healthcare provider about incorporating compression into your treatment plan. Your legs, and your life—will thank you.